Introduction
Neurogenic talipes equinovarus is a disease with the highest
prevalence and the greatest harm among the modern disabled
people. It is one of the common orthopedic malformations, and
also a disease with the longest treatment cycle, greater difficulty
and poor patient satisfaction. The main pathological change is
due to the dislocation of calcaneus, talus and scaphoid, which
leads to imbalance of muscle force and local tendon contracture.
It is a three-dimensional deformity caused by complex pathological changes of soft tissue and bone and joint, mainly manifested
as foot drop, high arch, varus, adduction and other foot and ankle
deformities. Due to the relative lack of subcutaneous soft tissue
and poor blood supply in the ankle, traditional surgery is easy to
cause skin ischemic necrosis, postoperative secondary infection,
soft tissue scar contracture and other complications, and the recurrence rate is as high as about 20% [1]. In order to reduce the
complications of correction of neurogenic talipes equinovarus and
reduce the recurrence rate after operation, we applied Ilizarov
technology for treatment. Lizarov technology is to install a special
external fixator in the ankle, and gradually correct the deformity
of horseshoe foot through slow tissue drafting. The clinical application of many scholars has proved that [2-3], not only the deformity correction is satisfactory, but also the shape and function
of the foot can be preserved to the maximum extent, and at the
same time, serious complications can be avoided and reduced.
It is a safe and reliable method for the correction of neurogenic
clubfoot. Due to the different treatment methods and various
methods, it is necessary to carry out personalized force line analysis, osteotomy plane and angle design, neuromyoelectric test and
analysis, determine tendon transposition, repair of nerve, blood
vessel and skin tissues, and long-term, systematic and comprehensive rehabilitation training after surgery according to the patient's different age, sex, occupation, deformity, etc. Therefore,
orthopedic physicians need to have comprehensive knowledge of
basic medicine and clinical medicine. However, at present, there
are not many orthopedic doctors who have received standardized training in China, and the amount of orthopedic operations is
large, with many therapeutic effects and postoperative complications. Therefore, this paper conducts a retrospective clinical study
on the treatment effect and postoperative complications of 182
patients with complete data from 262 patients with neurogenic
talipes equinovarus treated with Ilizarov technology in our hospital from January 2013 to December 2020.
Proposed methods
Inclusion criteria
(1) Foot deformity secondary to nervous system diseases, such
as cerebral palsy Poliomyelitis sequela, congenital horseshoe foot, etc;
(2) Type III (severe) or above according to Dimegl io classification method;
(3) No severe osteoporosis;
(4) Patients with complete clinical data and follow-up ≥ 3 times.
Exclusion criteria
(1) soft clubfoot;
(2) Plantar flexion deformity is less than 400 and there is no
complaint of discomfort; (3) Patients with incomplete clinical data and follow-up less than 3 times.
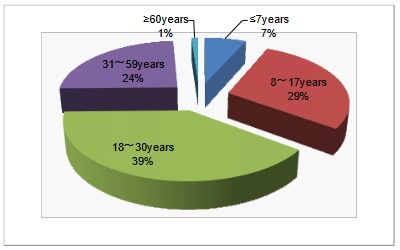
General data
182 patients (228 feet) in this group. Among them, 136 were
unilateral and 46 bilateral. 134 males (171 feet) and 48 females
(57 feet). The age ranged from 4 to 70 (  23.64 ± 13.96) years,
12 cases were ≤7 years old (6.6%), 52 cases were 8-17 years old
(28.6%), 72 cases were 18-30 years old (39.6%), 44 cases were
31-59 years old (24.2%), and 2 cases were ≥60 years old (1.1%)
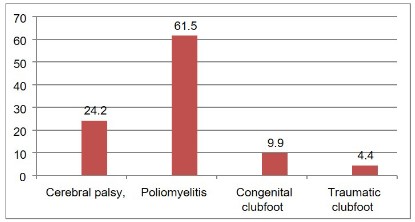
(Figure 1). Classification of diseases: 44 cases (24.2%) of sequelae
of cerebral palsy, 112 cases (61.5%) of sequelae of poliomyelitis,
18 cases (9.9%) of congenital clubfoot, and 8 cases (4.4%) of traumatic clubfoot Figure 2. Hospitalization time: 7~271 days (-83.19
± 43.8 days), return visits after discharge: 3~6 times (
23.64 ± 13.96) years,
12 cases were ≤7 years old (6.6%), 52 cases were 8-17 years old
(28.6%), 72 cases were 18-30 years old (39.6%), 44 cases were
31-59 years old (24.2%), and 2 cases were ≥60 years old (1.1%)
(Figure 1). Classification of diseases: 44 cases (24.2%) of sequelae
of cerebral palsy, 112 cases (61.5%) of sequelae of poliomyelitis,
18 cases (9.9%) of congenital clubfoot, and 8 cases (4.4%) of traumatic clubfoot Figure 2. Hospitalization time: 7~271 days (-83.19
± 43.8 days), return visits after discharge: 3~6 times (  3.4 ± 0.63
times).
3.4 ± 0.63
times).
Treatment method
According to the degree of bone deformity of the patient's foot,
muscle strength, age, the degree of cooperation of the patient
and his family, the ability of the doctor to master this technology and other factors, a personalized surgical plan is formulated.
First, according to the degree of deformity of the patient's foot,
the posterior medial soft tissue release, Achilles tendon lengthening, external transfer of tibial anterior muscle, osteotomy of the
three joints of the foot, internal rotation osteotomy under the
tibial tubercle and other soft tissue release, muscle force balance,
osteotomy correction and joint fusion were selected, and then
the Ilizarov external fixator was used for correction.
Data collection and sorting
During the hospitalization, the responsible physician (with
5-10 years of clinical experience) is responsible for tabulating, statistical analysis and sorting out the clinical symptoms, signs and
relevant examinations of patients after using the Ilizarov external
fixator. After the patient leaves the hospital, the responsible physician and the customer service department personnel will conduct telephone or on-site follow-up to the patient and his family
members 1 month, 3 months, 6 months, 1 year or 2 years after
the patient leaves the hospital. The responsible physician focuses
on understanding the patient's disease, guiding the later rehabilitation, prevention and treatment of complications, frame adjustment, frame removal, reexamination, etc. The customer service
department staff mainly understand the patient's recent situation, physical recovery, and the evaluation and suggestions on the
hospital's work.
Statistical methods
All data were analyzed by SPSS 20.0 software. The measurement data are expressed as mean ± standard deviation (

± S).
Take the percentage of 5 groups of data of the same variable, calculate the 99% confidence interval and the correlation between
the variables. The P value of the detection level is less than 0.05
on both sides, which is considered to be statistically significant.
Results and analysis
Evaluation method and efficacy
According to the ICFSG scoring standard, the patients were
scored according to the 2-year follow-up after surgery. 228 feet,
ICFSG score: excellent 136 feet, good 67 feet, fair 11 feet, poor 8
feet, the excellent and good rate is 89.04%
Postoperative complications and analysis
The time of using Ilizarov external frame for this group of cases
was 36~381 days (  86.3 ± 56.5).
86.3 ± 56.5).
The patients were followed up for 1 month, 3 months, 6
months, 1 year or 2 years after discharge.
The follow-up time ranged from 1 to 24 months, with an average of 16.2 months. Among them, 65 people (77 feet) had 16
kinds of complications, the incidence was 33.77%. It is significantly higher than 22.5% reported in the data [4]. We think it is
related to different statistical caliber. English literature records
the frequency of various complications during limb lengthening
of Ilizarov, which may reach 100% [5,6].
Early complications
In this group, 147 patients (178 feet) had pain, swelling, numbness and other symptoms after operation, accounting for 78.07%.
It lasted for 2~12 (  5.85 ± 2.41) weeks, 13 feet had needle infection, 17 feet had loose connecting rods, 5 feet had broken needles,
3 feet had nerve injury and 2 feet had skin necrosis. Needle infection is a common complication in the process of Ilizarov external fixation device orthopedics, with an incidence of 21%~42% [7-10].
The incidence of cases in this group is low (5.7%). The main causes
are thermal burns to tissues during operation, skin and muscle
injuries caused by long-term traction, exposed needle mouth pollution, and skin diseases of a few patients themselves. The causes
of this group of cases were prevented in advance, such as using
a protective sleeve when threading the needle during the operation, paying attention to the direction and strength of the steel
needle and the condition of skin displacement, ensuring the skin
is clean, and timely dealing with early infection. Therefore, the
needle infection rate is far lower than that reported in the literature. In this group, one patient suffered from allergic dermatitis
with infection and finally osteomyelitis due to untimely treatment
of early needle infection. The loose connecting rod is mainly due
to the loose screw fixation or more patient activities, especially in
the rehabilitation training of patients with spastic cerebral palsy.
In order to relieve local tension pain, individual patients adjust
the screw by themselves. Two cases of common peroneal nerve
injury and one case of posterior tibial nerve injury were caused
by intraoperative traction. After the application of neurotrophic
drugs, rehabilitation physiotherapy and other treatments, they all
recovered completely. Two patients suffered from skin necrosis
within 1 cm around the anterior medial tibial needle path due
to skin heat injury, and recovered after dressing change. 5. The
needle breaks at the edge of the fixed screw. Pull out the broken
end and fix the broken pin again with the connecting piece, which
does not affect the fixing effect.
5.85 ± 2.41) weeks, 13 feet had needle infection, 17 feet had loose connecting rods, 5 feet had broken needles,
3 feet had nerve injury and 2 feet had skin necrosis. Needle infection is a common complication in the process of Ilizarov external fixation device orthopedics, with an incidence of 21%~42% [7-10].
The incidence of cases in this group is low (5.7%). The main causes
are thermal burns to tissues during operation, skin and muscle
injuries caused by long-term traction, exposed needle mouth pollution, and skin diseases of a few patients themselves. The causes
of this group of cases were prevented in advance, such as using
a protective sleeve when threading the needle during the operation, paying attention to the direction and strength of the steel
needle and the condition of skin displacement, ensuring the skin
is clean, and timely dealing with early infection. Therefore, the
needle infection rate is far lower than that reported in the literature. In this group, one patient suffered from allergic dermatitis
with infection and finally osteomyelitis due to untimely treatment
of early needle infection. The loose connecting rod is mainly due
to the loose screw fixation or more patient activities, especially in
the rehabilitation training of patients with spastic cerebral palsy.
In order to relieve local tension pain, individual patients adjust
the screw by themselves. Two cases of common peroneal nerve
injury and one case of posterior tibial nerve injury were caused
by intraoperative traction. After the application of neurotrophic
drugs, rehabilitation physiotherapy and other treatments, they all
recovered completely. Two patients suffered from skin necrosis
within 1 cm around the anterior medial tibial needle path due
to skin heat injury, and recovered after dressing change. 5. The
needle breaks at the edge of the fixed screw. Pull out the broken
end and fix the broken pin again with the connecting piece, which
does not affect the fixing effect.
Late complications
The application of Ilizarov technology has created unique technical advantages for limb orthopedics, but there may be a variety
of complications in the application of Ilizarov technology, including needle infection, osteomyelitis, foot swelling, toe flexion deformity, metatarsophalangeal joint subluxation, foot stiffness and
even recurrence [11-13]. It is difficult to treat adult neurogenic
talipes equinovarus, especially in patients with long course and
severe deformity. Although there are many methods of surgical
treatment, it is difficult to correct all malformations in one operation [14]. Repeated soft tissue release and osteotomy orthopaedic surgery are more likely to cause stiffness, small and pain of
the foot and ankle [15,16]. Beaty JH. Freedman JA et al. [12,13]
believed that ankle and subtalar joint stiffness, arthritis, pain and
residual deformity existed for a long time. In this group, 1.8% of
the patients had limited knee movement, 2.6% had ankle arthritis and 1.3% had subtalar joint stiffness, which was lower than
that reported in the literature. The deformity of toe flexion contracture was 5.7%. After orthopedic surgery, a kind of instinctive
anti fall reflex causes the toe to flex and contract for a long time
when the foot touches the ground, resulting in toe flexion contracture deformity. Parmanand Gupta et al., [17] believed that toe
flexion contracture deformity is a complication that is difficult to
treat, and once it occurs, it will not be able to participate in sports
competitions as a professional athlete. In this group, 43 patients
(49 feet) had limb pain, swelling, numbness and other symptoms
more than 3 months after surgery, which we call "tissue displacement syndrome", accounting for 21.49%. The incidence of complications in different age groups is shown in table 1.
Table 1: Postoperative complications at different ages.
| complication |
year |
year |
year |
year |
year |
Total (%) |
| Pain (>3 months) |
1 |
2 |
12 |
9 |
1 |
25 (10.96) |
| Swelling (>3 months) |
1 |
2 |
10 |
9 |
1 |
23 (10.09%) |
| Numbness (> March) |
1 |
5 |
16 |
12 |
1 |
35 (15.35%) |
| Needle infection |
1 |
1 |
5 |
6 |
0 |
13 (5.7%) |
| Broken needle |
0 |
0 |
2 |
3 |
0 |
5 (2.2%) |
| Loose connecting rod |
1 |
2 |
6 |
8 |
0 |
17 (7.5%) |
| osteomyelitis |
0 |
0 |
1 |
0 |
0 |
1 (0.4%) |
| Restricted knee movement |
0 |
0 |
2 |
2 |
0 |
4 (1.8%) |
| Nonunion of bone |
0 |
0 |
1 |
1 |
0 |
2 (0.9%) |
| Skin necrosis |
0 |
1 |
0 |
1 |
0 |
2 (0.9%) |
| Nerve injury |
0 |
0 |
1 |
1 |
0 |
3 (1.3%) |
| Ankle dislocation |
0 |
0 |
2 |
1 |
0 |
3 (1.3%) |
| Toe flexion deformity |
1 |
3 |
5 |
4 |
0 |
13 (5.7%) |
| recrudescence |
0 |
1 |
1 |
1 |
0 |
3 (1.3%) |
| Ankle arthritis |
0 |
0 |
3 |
3 |
0 |
6 (2.6%) |
| Subtalar joint stiffness |
0 |
0 |
2 |
1 |
0 |
3 (1.3%) |
Tissue displacement syndrome
The clinical characteristics of equinovarus foot are mainly ankle
plantar flexion, heel varus and forefoot adduction [18]. During the
surgical correction, tendon transposition, such as Achilles tendon
extension and tibial anterior tendon insertion, should be done.
A few patients need to do rectangular shortening osteotomy of
the lateral column of the calcaneus, then use a steel needle to
cross the calcaneus and metatarsal, connect the half ring and fix
it on the calcaneus and foot back, and then slowly pull it for 2 to
3 months, so that the forefoot and midfoot gradually rotate out-ward and turn outward, so as to restore the normal appearance
of the foot. During the whole operation and slow tissue traction
process, the tissue has been displaced, local micro vessels have
been damaged, and circulation obstacles have occurred, leading to local swelling; Pain caused by tissue injury, hemorrhage,
edema, and inflammatory stimulation; Tissue compression, nerve
damage, numbness. This series of pathophysiological reactions is
called "tissue displacement syndrome". The similar reaction in the
earlier stage is "tissue displacement reaction". If the angle of the
external frame is adjusted properly or the speed of frame adjustment is slowed down, drug treatment, physical therapy and other
comprehensive treatments are carried out, and the symptoms still
have no significant change and affect the normal walking function
after more than 3 months, it is called "tissue displacement syndrome". The severity of the syndrome is related to surgical trauma, displacement angle, traction time, speed, patient age, and
body regeneration and repair ability. In this group, most of the
patients with "tissue displacement syndrome" occurred in adults
over 18 years old, and there was a significant positive correlation
with age (P<0.05-0.01). Among the 43 patients with "tissue displacement syndrome" in this group, 26 (60.47%) were followed
up 1 year after discharge, and 12 (27.91%) were followed up 2
years after discharge. The symptoms such as swelling and pain of
the patients' limbs basically disappeared, and some patients felt a
little numbness locally, but the walking function of the limbs was not affected. Five patients were not followed up. The symptoms
of patients with "tissue displacement syndrome" persist, but the
prognosis is good.
Correlation between complications and age
The correlation test was conducted between the first 6 complications with high incidence rate and different age variables.
Among them, pain, swelling and numbness (tissue displacement
syndrome) were positively correlated with age (P<0.05-0.01). There was no correlation between needle infection, loose connecting rod and toe flexion deformity and age (P>0.05) table 2.
Table 2: Correlation between major complications and different
age variables.
| Age
year |
Pain |
Swelling |
Numbness |
Needle
infection |
Loose
connecting rod |
toe flexion
deformity |
| ≤ 7 |
0.832 |
0.83 |
0.83 |
8.3 |
8.3 |
8.3 |
| 8~17 |
3.85 |
3.85 |
9.62 |
1.9 |
3.8 |
5.8 |
| 18~30 |
16.67 |
13.89 |
22.22 |
6.9 |
8.7 |
6.9 |
| 31~59 |
20.45 |
20.45 |
27.27 |
13.6 |
18.2 |
9.1 |
| ≥ 60 |
50.00 |
50.00 |
50.00 |
0 |
0 |
0 |
| r |
0.93 |
0.926 |
0.976 |
-0.144 |
0.51 |
-0.585 |
| p |
<0.55 |
<0.55 |
<0.01 |
>0.55 |
>0.55 |
>0.55 |
Prevention measures
The distraction osteogenesis theory of Ilizarov technology has
proved that the external fixator is beneficial to the shape recovery
of various bone tissues, the adjustment and maintenance of limb
length during the slow traction process, so that the correction of
talipes equinovarus deformity can obtain satisfactory results for
clinicians and patients [18,19]. However, due to the wide variety
of configurations of external fixation devices, wide surgical indications, and long learning curve of postoperative management process and doctors, errors are inevitable in the treatment process,
and problems in any link, such as needle threading and installation
of external fixators, needle bag, postoperative management and
guidance of patients' functional training, and the time to remove
external fixators, may occur large and small complications [4].
However, through our efforts, most of these complications can be
avoided. Paley [20] divided the problems arising from the application of Ilizarov technology into three categories: one is called
problems, which can be solved without surgery; The second type
is called obstacle, which needs to be solved by reoperation, but
will not leave sequela; The three types are called complications,
which will still leave morphological abnormalities or dysfunction
after treatment. According to the Paley classification, there are
6 kinds of "problems" in this group, of which 3 are "tissue displacement syndrome"; 6 "obstacles"; There were 4 kinds of "complications", 25 feet, accounting for 10.96%. Orthopedic surgery
(including peripheral nerve surgery) is recommended by the bone
and joint professional committee of the Chinese Rehabilitation
Medical Association, the China Brain Palsy Multidisciplinary Co-operation Alliance, and the surgical treatment experts of spastic
cerebral palsy by consensus as the second stage surgery of spastic
cerebral palsy, an important supplement to SPR surgery, and is
not recommended to take corrective surgery first. It is suggested
that rehabilitation training is an important guarantee for postoperative functional improvement. Advocate the concept of "three
points operation, seven points training" [21]. Therefore, the key
to the successful treatment of neurogenic clubfoot is to objectively predict the surgical effect, fully communicate with patients,
reduce patients' expectations, improve patients' compliance,
strengthen the sense of responsibility of medical personnel, scientifically, rigorously and strictly control the surgical indications,
reduce complications, strengthen long-term and standardized rehabilitation training for patients after surgery, and cooperate with
doctors and patients.
Conclusion
In this group, 182 patients (228 feet) with neurogenic clubfoot
were treated with Ilizarov external fixator, and the excellent and
good rate was 89.04%. There were 16 kinds of complications, accounting for 33.77%. In the early stage, pain, swelling, numbness
and other "tissue displacement reactions" were the main symptoms (78.07%). In the later stage, "tissue displacement syndrome"
occurred (21.49%), but the prognosis was good. Among them,
88.37% of the patients had basically recovered from follow-up
data within two years. The loose connecting rod accounted for
7.5%, toe flexion deformity and needle infection accounted for
5.7% respectively. The main complications increased with age,
and there was a significant positive correlation between complications and age (P<0.05). However, through our efforts, most of
these complications can be avoided. Therefore, in the process of
applying Ilizarov technology to correct neurogenic talipes equinovarus, we should strengthen the sense of responsibility of medical personnel and improve their professional skills. Scientific, rigorous and strict control of surgical indications. Do a good job of
communication between doctors and patients before surgery to
improve patients' compliance with treatment. Personalized installation and adjustment of the external frame, strengthening longterm postoperative rehabilitation training, and other factors are
the key to reduce complications and successfully treat neurogenic
clubfoot.
Declarations
Data availability: The data used to support the study are included in the paper.
Conflicts of interest: The authors declare that there are no
conflicts of interest.
References
- Bradish CF, Noor S. The Ilizarov method in the management of relapsed club feet. J Bone Joint Surg( Br). 2000; 82: 387-391.
- Ferreira RC, Costo MT, Frizzo GG, da Fonseca Filho FF. Correction
of neglected clubfoot using the Ilizarov external fixator. Foot AnkleInt. 2006; 4: 266-273.
- Prem H, Zenios M, Farre lR, Day JB. Soft tissue Ilizarov correction of
congenital talipes equinovarus 5to 10 years post surgery. J Pediatr
Orthop. 2007; 2: 220- 224.
- Jiao Shaofeng, Qin Sihe. Analysis of complications of Ilizarov technique in the treatment of limb deformity. Chinese Journal of Orthopedics. 2012; 32: 245-248.
- Hosny GA. Limb lengthening history, evolution, complications and
current concepts. J Orthop Traumatol. 2020; 21: 3.
- Liu Y, Yushan M, Liu Z, Liu J, Ma C, et al. Complications of bone
transport technique using the Ilizarov method in the lower extremity: a retrospective analysis of 282 consecutive cases over
10 years. BMC Musculoskelet Disord. 2020; 21: 354.
- Hassan A, Letts M. The management of the neglected congenital
foot deformity in the older child with the Taylor spatial frame. J
Pediatr Orthop. 2012; 32: 85-92.
- Mahan J, Seligson D, Henry SL, Hynes P, Dobbins J. Factors in pin
tract infections. Orthopedics. 1991; 14: 305-308.
- Ahlborg HG, Josefsson PO. Pin-tract complications in external fixation of fractures of the distal radius. Acta Orthop Scand. 1999; 70:
116-118.
- Camathias C, Valderrabano V, Oberli H. Routine pin tract care in external fixation is unnecessary: A randomized prospective blinded
controlled study. Injury. 2012; 43: 1969-1973.
- Grill F, Franke J. The Ilizarov distractor for the correction of relapsed or neglected clubfoot. J Bone Joint Surg Br. 1987; 69: 593-
597.
- Beaty JH. Congenital clubfoot (talipes equinovarus). In: Canale ST,
editor. Campbell’s operative orthopedics. 10th ed. Philadelphia,
PA: Mosby; 2003; 988-1006.
- Freedman JA, Watts H, Otsuka NY. The Ilizarov method for the
treatment of resistant clubfoot: is it an effective solution? J Pediatr
Orthop. 2006; 26: 432-437.
- Al-Raggad M. Talectomy in the treatment of resistant talipes
equinovarus deformity: the indications and result. International
Journal of Biological and Medical Research. 2013; 4: 3642-3644.
- Ippolito E, Farsetti P, Caterini R, Tudisco C. Long-term comparative
results in patients with congenital clubfoot treated with two different protocols. J Bone Joint Surg Am. 2003; 85: 1286-1294.
- Dobbs MB, Nunley R, Schoenecker PL. Long-term follow-up of patients with clubfeet treated with extended soft tissue release. J
Bone Joint Surg Am. 2006; 88: 986-996
- Parmanand Gupta, Nitin Bither. Ilizarov in relapsed clubfoot: a necessary evil? Journal of Pediatric Orthopaedics B. 2013; 22: 589-
594.
- Wallander HM. Congenital clubfoot. Aspects on epidemiology,
residual deformity and patient reported outcome. Acta Orthop
Suppl. 2010; 81: 1-25.
- El-Sayed M, Ilizarov external fixation for management of severe relapsed clubfeet in older children. Foot Ankle Surg. 2013; 19: 177-
181.
- Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res.1990; 2501:
81-104.
- Professional Committee of Bone and Joint of China Rehabilitation
Medical Association, China Association for Multidisciplinary Collaboration of Cerebral Palsy, and consensus of surgical treatment
experts for spastic cerebral palsy. Chinese Journal of Orthopedics.
2020; 28: 77-81.