Introduction
Classic aorto-coronary bypass is performed under conditions
of extracorporeal circulation (Ecc), on a systolic heart. Cardiopulmonary By-Pass (CPB) is a method by which heart action and
pulmonary circulation are replaced during cardiac surgery. The
main role of this technique is to ensure tissue oxygenation and
thermoregulation during surgical intervention. For this purpose, a
machine for extracorporeal circulation is used [1].
Cardiopulmonary bypass allows the patient’s heart and lungs
to be temporarily isolated from circulation and their activity suspended so that cardiac surgery intervention can be performed
under controlled conditions. The most common material for making extracorporeal blood flow systems is Polyvinyl Chloride (PVC),
but silicone and latex rubber are also used [2]. Anticoagulation
is necessary so that the patient can be safely connected to the
extracorporeal circulation machine during cardiac surgery. The
contact of blood and artificial non-biological surfaces of the extracorporeal blood flow system leads to the activation of the coagulation system and the formation of a clot in the circulation within
a few minutes in the absence of anticoagulant drugs. Inadequate
anticoagulation in its most serious form leads to a lethal outcome,
and in a milder form leads to kidney or brain dysfunction. The
most commonly used anticoagulant is High Molecular Weight
Heparin (HMH).
Bleeding during and after cardiopulmonary by-pass is multifactorial. Namely, the prolonged contact of platelets with the plastic
hoses of the extracorporeal blood flow system disrupts their function, leads to the activation of platelets and the coagulation cascade, which ultimately results in thrombocytopenia by more than
30%, as well as consumptive coagulopathy. Contact activation of
the coagulation cascade occurs when the artificial surface of the
intestine comes into contact with blood, primarily through the activation of factor XII. Platelets of patients who undergo cardiac
surgery are very sensitive, because patients are usually preoperatively on mono or dual antiplatelet therapy, which inhibits their
function and additionally disrupts perioperative and postoperative hemostasis. Dilution as part of priming, hypothermia during
the intervention, extended duration of the extracorporeal blood
flow procedure, also disrupt systemic hemostasis. A certain number of patients are on oral or parenteral anticoagulation therapy
before surgery, which prevents successful hemostasis by inhibiting the activation of factors II, VII, IX, X, XI. Increased perioperative blood loss, combined use of heparin and protamine, preoper-
ative anemia, renal insufficiency, liver disease, age over 70 years,
female sex, congenital or acquired coagulopathies are all risk factors that disturb the coagulation cascade and hemostasis [4,5].
Due to all of the above, one of the most difficult tasks in cardiac surgery is the establishment of timely, physiological hemostasis. Bleeding usually occurs during and after cardiac surgery.
During such an emergency, routine laboratory testing of coagulation using PT, APTT, platelet count is usually slow and insufficient.
Point of Care (POC) devices for monitoring the hemostasis system,
and above all rotational thromboelastometry [6], play a real role
in the aforementioned acute conditions.
Systemic hemostasis therapy is of crucial importance for the
timely management of bleeding complications, and proper antiplatelet and anticoagulant therapy for the prevention of thrombosis [7].
Materials and methods
This retrospective study included 100 patients who underwent
single, double and triple surgical revascularization of the myocardium, at the Clinic for Cardiac Surgery of Clinical center Niš Serbia,
over a period of 6 months. 100 respondents were included in the
research (22 female respondents - 22.0% and 78 male respondents - 78.0%). The average age of the studied population is 64.6
± 7.5 years (Min 43, Max 80 years).
After standard cardiac surgical preoperative preparation of patients, patients were operated according to standard cardiac surgical protocols.
Preoperatively, as well as 3 hours and 24 hours postoperatively,
the following parameters were determined:
1. Blood count (erythrocyte count-Rbc, hemoglobin-Hgb,
hematocrit-Hct, leukocyte count-Wbc, platelet count-Plt) on a
Horiba CRP 200 automatic counter, from 4ml whole blood sampled in a tube with EDTA anticoagulant.
2. Coagulation status (prothrombin time-PT, International Normalized Ratio-INR, activated partial thromboplastin time-aPTT,
fibrinogen-F I, antithrombin III-AT III, D dimer, on the ACL Elite Pro
device, from whole blood taken in a tube with Na-citrate as an
anticoagulant, which was centrifuged for 15 min at 3500 revolutions immediately after sampling, and then 250 microliter samples pipetted from the serum were allowed to be tested on the
coagulometer.
4. Basic parameters of thrombelastometry (parameters of the
internal-IN test and the external coagulation pathway-EX test,
namely: (coagulation time-CT which depends on the concentration and activity of coagulation factors in plasma, maximum clot
strength-MCF whose value is determined by the number and by
platelet function as well as fibrinogen concentration, clot amplitude after 10 minutes-A10 also depends on platelet count/function and fibrinogen concentration, alpha angle, maximum lysis-ML
which registers pathological clot lysis), functional fibrinogen-FIB test, A10 which depends on persistence and fibrin clot polymerization), on a rotary thromboelastometer device Clot pro, Enicor,
Germany, from whole blood 4 ml in a test tube with sodium citrate as an anticoagulant, and the blood was also analyzed within
30 minutes of sampling.
5. The use of blood and blood products, perioperatively and
postoperatively, is recorded in the medical documentation that is
kept in the operating room (operative list), as well as in the intensive care unit (intensive care unit list).
6. The use of synthetic hemostasis agents (prothrombin complex concentrate-PCC, desmopressin-acetate-DDAVP, tranexamic
acid) was recorded in the medical documentation kept in the operating room (operation list) as well as in the intensive care unit
(shock list).
7. Use of autotransfusion through the Haemonetics Cell Saver
5+ intraoperative blood saving device, the amount of perioperative bleeding (recorded in the operating room-saver list) and
postoperative bleeding through drains in the intensive care unit
(shock list) was monitored.
The basic parameters of Clot pro tests that are related to various disorders of hemostasis (accompanied by increased bleeding)
and the consequent application of hemostasis therapy are:
- Coagulation time-CT Ex test≥100 s (ref. value 38-79 s), indicates disorder of the coagulation factor of the external coagulation pathway (II, V, VII, IX factor).
- Coagulation time-CT In test≥300 s (ref. value 100-240 s), refers to the disruption of the coagulation factors of the internal
pathway (all factors except VII and XIII) or the presence of the
residual effect of high molecular weight heparin.
- Maximum clot strength-MCF Ex test/In test ≤45 mm (ref.
value 50-72 mm), occurs with impaired function and number of
platelets or with fibrinogen deficiency. Clot amplitude after 10
minutes-A10 Fib test≤8 mm (ref. value 9-23 mm) is registered with
low concentration and poor polymerization of fibrin clot, which
depends on the concentration of functional fibrinogen.
-Maximum clot lysis-ML≥15% (ref.value <15%) indicates pathological hyper fibrinolysis, which also results in increased bleeding
in patients.
Statistical data processing
The data are presented in the form of arithmetic mean and
standard deviation, minimum and maximum values, as well as in
the form of absolute and relative numbers.
The normality of continuous variables was tested with the
Kolomogor-Smirnov test. If the distribution of the data was normal, the comparison of values preoperatively and postoperatively
in two moments (3 h and 24 h after the operation) was performed
with the ANOVA test for repeated measurements. If the data
distribution is not normal, the Friedman test was used for this
comparison. If the data distribution is normal, the comparison between the two groups was performed using the t test, if the data
distribution is not normal, this comparison was performed using
the Mann-Whitney test.
The hypothesis was tested with a significance threshold of p<0.05. Data analysis was performed in the SPSS 16.0 software
package.
Results
The number of erythrocytes monitored in three measure-
ments decreases statistically significantly (p<0.001). Also, hemoglobin and hematocrit values decrease statistically significantly in
the monitored period (p<0.001 and p<0.001, respectively). The
number of leukocytes increases after 3 hours from the operation
compared to the period before the operation, and then decreases
up to 24 hours after the operation. A statistically significant difference was found in the number of leukocytes in the monitored
period (p<0.001). Platelets drop sharply up to 3 hours after the
operation, then in the period of 24 hours after the operation we
have a slight increase. The number of platelets changes statistically significantly during the follow-up period (p<0.001) (Table 1).
Table 1: Values of Erythrocytes (RBC), Hemoglobin (HGB), Hematocrit (Hct), leukocytes (Wbc) and Platelets (PLT) measured preoperatively and postoperatively after 3h and 24h.
| Parameter |
Preoperatively |
3h postoperatively |
24 h postoperatively |
p-value1 |
| RBC (1x1012) |
4,46 ± 0,47 |
3,86 ± 0,55 |
3,76 ± 0,49 |
<0,001 |
| Hgb (g/dl) |
137,74 ± 10,93 |
114,98 ± 11,32 |
109,96 ± 8,87 |
<0,001 |
| Hct (%) |
39,18 ± 4,17 |
32,99 ± 3,95 |
31,86 ± 3,10 |
<0,001 |
| WBC (1x109) |
7,11 ± 1,28 |
10,07 ± 3,07 |
9,14 ± 3,34 |
<0,0012 |
| PLT (1x109) |
236,22 ± 63,88 |
148,13 ± 56,65 |
167,01 ± 50,96 |
<0,0012 |
⸶Arithmetic mean±standard deviation, 1 ANOVA for repeated measures,
2 Friedman's test.
Table 2: Values of PT, INR, aPTT, F I, AT III and D-dimer measured
preoperatively and postoperatively after 3h and 24h.
| Parameter⸶ |
Preoperatively |
3h postoperatively |
24 h postoperatively |
p-value1 |
| PT (s) |
11,67 ± 1,47 |
15,81 ± 5,22 |
12,63 ± 1,42 |
<0,001 |
| INR |
1,15 ± 0,13 |
1,57 ± 0,55 |
1,26 ± 0,14 |
<0,001 |
| Aptt (s) |
28,03 ± 3,78 |
34,28 ± 13,26 |
30,36 ± 6,82 |
<0,001 |
| F I (g/L) |
4,14 ± 1,40 |
3,16 ± 1,25 |
4,40 ± 1,00 |
<0,001 |
| ATIII (%) |
89,26 ± 12,46 |
70,38 ± 10,78 |
68,27 ± 8,36 |
<0,001 |
| D dimer (ng/ml) |
500,30 ± 1028,32 |
611,35 ± 1012,42 |
581,32 ± 968,39 |
0,0892 |
⸶Arithmetic mean±standard deviation, 1 ANOVA for repeated measures,
2Friedman's test.
PT increases 3 hours after surgery, and then decreases by 24
hours. It was found that there was a statistically significant difference in PT in the follow-up period (p<0.001). The INR increases 3
hours after the operation, and then falls by 24 hours. It was found
that there was a statistically significant difference in INR during
the follow-up period (p<0.001).
APTT increases 3 hours after surgery, and then falls by 24
hours. It was found that there was a statistically significant difference in APTT in the follow-up period (p<0.001).
The values of fibrinogen (F I) decrease in the first 3 hours after
the operation, and then in the period up to 24 hours after the operation, they return to the values that were before the operation.
It was found that there is a statistically significant difference in F I
values in three measurements (p<0.001).
The values of antithrombin three (ATIII) decrease statistically
significantly in three measurements (p<0.001).
D dimer in the period of 3 hours after the operation increases
compared to the preoperative values, and then in the period up
to 24 hours after the operation it slightly decreases. It was found
that the values of D dimer do not change statistically significantly
in three measurements (p=0.089) (Table 2).
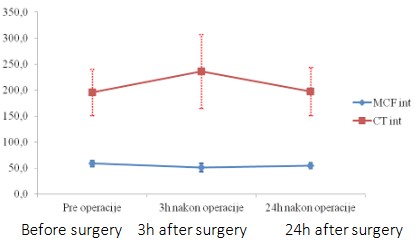
Table 3: Values of CT int and MCF int in the follow-up period in the
studied population.
| Parameter⸶ |
Preoperatively |
3h postoperatively |
24 h postoperatively |
p-value1 |
| CT IN test (s) |
195, 96 ± 44,63 |
236, 11 ± 70,65 |
197, 43 ± 46,83 |
<0,001 |
| MCF IN test (mm) |
58, 89 ± 5,70 |
50, 91 ± 7,87 |
54, 70 ± 7,87 |
<0,001 |
⸶Arithmetic mean ± standard deviation, 1Friedman’s test.
CT in test values increase in the first 3 hours after the operation
compared to the preoperative period, and then return to preoperative values in the period up to 24 hours. It was found that there
is a statistically significant difference in CT in test values between
the three measurements (p<0.001) (Table 3). MCF in test values
fall in the first 3h after surgery compared to the preoperative period, and then begin to increase slightly in the period up to 24h
after surgery. It was found that there is a statistically significant
difference in the values of this parameter between the three measurements (p<0.001) (Table 3, Graph 1).
Ex test CT values increase in the first 3 hours after the operation compared to the preoperative period, and then in the period
up to 24 hours they fall to lower values compared to the preoperative period. It was found that there is a statistically significant
difference in CT extem values between the three measurements
(p<0.001) (Table 4). MCF ex test values fall in the first 3 hours after
surgery compared to the preoperative period, and then begin to
rise slightly in the period up to 24 hours after surgery. It was found
that there is a statistically significant difference in the values of
this parameter between the three measurements (p<0.001) (Table 5, Graph 2).
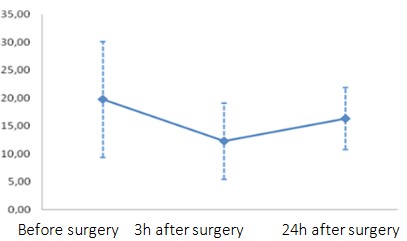
A10 fib test values decrease up to 3 hours after surgery (12.31
± 6.82) compared to preoperative values (19.79 ± 10.35), and then
a slight increase begins (16.36 ± 5.89) (Graph 3). It was found that
there is a statistically significant difference in the values of this
parameter between the three measurements (p<0.001).
A10 fib test values decrease up to 3 hours after surgery (12.31
± 6.82) compared to preoperative values (19.79 ± 10.35), and then
a slight increase begins (16.36 ± 5.89) (Graph 3). It was found that
there is a statistically significant difference in the values of this
parameter between the three measurements (p<0.001).
Table 5: Parameters indicating increased peri and postoperative
bleeding.
|
Preoperatively |
3h postoperatively |
24 h postoperatively |
| CT ex test>100 (s) |
0 (0,0%) |
4 (4,0%) |
0 (0,0%) |
| MCF ex test<45 (mm) |
0 (0,0%) |
21 (21,0%) |
3 (3,0%) |
| CT in test>300 (mm) |
0 (0,0%) |
23 (23,0) |
0 (0,0%) |
| MCF in test<45 (mm) |
0 (0,0%) |
17 (17,0) |
5 (5,0%) |
| A10 fib test≤8 (mm) |
8 (8,0%) |
15 (15,0%) |
2 (2,0%) |
| INR>2 |
0 (0,0%) |
6 (6,0%) |
0 (0,0%) |
| APTT>50 (s) |
0 (0,0%) |
8 (8,0%) |
5 (5,0%) |
| ML>15 (%) |
0 (0,0%) |
0 (0,0%) |
0 (0,0%) |
Four patients (4.0%) had CTextem greater than 100 3 hours after surgery.
Four patients (4.0%) had CTextem greater than 100 3 hours after surgery.
21 patients (21.0%) had MCFextem less than 45 3 hours after surgery and
3 patients (3.0%) 24 hours after surgery.
Table 6: Postoperative bleeding in relation to low values of MCF
ex test parameters.
| Time of measeurements |
MCF ex |
Postoperative bleeding |
|
AS ± SD |
p-value1 |
| 3 h after surgery |
<45 (mm) |
1988,10 ± 1083,73 (ml) |
0,001 |
| ≥45 (mm) |
1317,09 ± 326,293 (ml) |
|
⸶Arithmetic mean ± standard deviation, 1Man-Whitey test.
Bleeding after surgical intervention is statistically significantly
higher in patients who had MCF ex test <45 mm 3 h after surgery
(p<0.001) (Table 6).
Table 7: Postoperative bleeding in relation to low values of MCF
in test parameters.
| Time of measeurements⸶ |
MCF int |
Postoperative bleeding |
|
AS ± SD |
p-value1 |
| 24h after surgery |
<45 (mm) |
3550,00 ± 1286,47 (ml) |
0,002 |
| ≥45 (mm) |
1347,89 ± 319,73 (ml) |
|
⸶Arithmetic mean ± standard deviation, 1Man-Whitey test.
Postoperative bleeding is statistically higher in patients who
had MCF in test <45 mm 24 hours after surgery (p=0.002) (Table
7).
Discussion
It is important to note that in the majority of patients who underwent cardiac surgical procedures and who had an increased
rate of morbidity and mortality, an average of one to two units of
blood was given. These patients are mainly treated for anemia,
but in principle they were hemodynamic [8].
The study we conducted included 100 cardiac surgery patients,
of which 20 patients received an average of one unit - 350 ml of
resuspended erythrocytes within 24 hours postoperatively, exclusively for Hgb values ≤85 g/l, with the aim of correcting postoperative anemia in order to avoid hypoxia, which is in accordance
with the previously described results.
Thromboelastography is a dynamic qualitative and quantitative
assessment of clot formation that consists of three phases: clot
initiation, clot firmness and clot stability (fibrinolysis). Performing
thromboelastography using Clot Pro is very useful, but they do
not eliminate the need for other POC techniques that allow the
evaluation of platelet function (eg Aggregometry-Multiplate), all
of which are incorporated in numerous algorithms that are constantly being modified and developed [9].
Despite the improvements achieved with existing new techniques, most surgeons still tend to accept a significant amount
of blood loss as a characteristic of cardiac surgery [10]. Research
conducted in our institution also indicates that only 9% of patients
had an average postoperative drain loss of more than 1000 ml,
primarily thanks to the timely application of hemostatic agents,
the so-called Targeted hemostasis therapies guided by point of
care devices for hemostasis testing.
It is very important to ensure adequate drainage and removal
of blood from the pericardium and pleura (it has high fibrinolytic
activity and tissue coagulation factor). Removal of this blood and
clot likely not only reduces the chance of excessive blood loss by
preventing systemic coagulopathy, but is likely to have beneficial
effects on several other factors associated with surgery such as inflammation, atrial fibrillation, pericardial effusions (tamponade),
and the development of adhesions. Our results indicate that not a
single patient was registered with pathological hyperfibrinolysis,
which is a consequence of the early administration of the antifibrinolytic-tranexamic acid in a dose of 1000 mg immediately after
sternotomy.
After careful evaluation, it seems that hemodilution is the most
pronounced factor associated with the development of coagulopathy after cardiac surgery, and probably plays an important role
in the occurrence of blood loss after heart surgery. Prothrombin
complex concentrate (PCC) is a hemostatic agent that is applied in
case of deficiency of vitamin K-dependent coagulation factors (II,
VII, IX, X), which occurs especially in dilutional coagulopathy during and after cardiac surgery. The advantage is on the side of PCC
compared to plasma. Currently, there is no consensus on the dosage and timing of PCC administration, and the increased risk of
thromboembolic complications must always be balanced for PCC
administration. Three patients in this study received PCC post-operatively with an average of 1000 i.u. due to the deficit of the
mentioned factors, which was registered through the parameter
CT≥100 s ex test on Clot Pro, as well as prothrombin time values,
i.e. INR over 5.
Fibrinogen is one of the most important factors of coagulation,
and it is possible that the clotting process falls below the critical
level during hemodilution, so care should be taken and, if necessary, administration of fibrinogen concentrate [11]. Given that we
did not have fibrinogen concentrate, following the values of the
Fib test on Clot Pro, and especially the amplitude of the clot after
10 minutes (A10), 13 patients received cryoprecipitate early post-operatively (within 3 hours after the intervention) in an average
of 15 doses per patient.
The use of POC evaluation can provide faster and more complete insight into this delicate balance, creating a more individualized treatment oriented towards each patient separately. A large
variation in the sensitivity of the patient to the use of clopidogrel
often gives very different individual results before surgery, which
requires further use and determination of POC before, during and
after cardiac surgery. An individual approach oriented towards
each patient can contribute to the reduction of perioperative and
postoperative blood loss and reduce the need for transfusion to
a minimum [12].
Conclusion
Due to the complexity and duration of cardiac surgery, pronounced hemostatic changes occur in patients undergoing CABG.
Because of all of the above, the priority is to diagnose the most
common coagulation disorders in patients who have undergone
surgical revascularization of the myocardium and to choose an
adequate hemostasis therapy for the timely management of coagulation disorders in cardiac surgery patients.
Devices for POC testing of the hemostasis system have a special
clinical significance, with the use of which the correct and timely
diagnosis of the mentioned coagulation disorders, the prediction
of possible bleeding that has not yet manifested itself clinically, as well as the choice of targeted hemostasis therapy that will prevent or stop bleeding, is enabled.
It should be noted that 20% of patients after cardiac surgery
received a transfusion of resuspended erythrocytes (on average
1 unit), and all operated patients received an autologous transfusion of their own blood during the intervention via an intraoperative blood rescue device.
Due to all of the above, only 9% of surgical patients had a drainage of more than 1 L in the first 24 hours after surgery, without
any complications in terms of surgical reintervention.
Modern methods in combination with proven clinical protocols, great clinical experience of the staff, respecting the principle
"time is life", enable the best possible care of patients with detected hemostasis disorder in cardiac surgery.
References
- Herzog CA, Ma JZ, Collins AJ. Comparative survival of dialysis patients in the United Statesafter coronary angioplasty, coronary
artery stenting, and coronary artery bypass surgery andimpact of
diabetes. Circulation. 2002; 106: 2207-2211.
- Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, et al. Guidelines on themanagement of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pec-
toris of the European Society of Cardiology. Eur Heart J. 2006; 27:
1341-1381.
- Trullàs JC, González-Franco Á. Major developments in the 2016
european guidelines for heart failure. Rev Clin Esp. 2017; S0014-2565: 30052-30058.
- Fuster V, Moreno PR, Fayad ZA, Corti R, Badimon JJ, et al. Atherothrombosis and high-risc plaque: part I: evolving concepts. J Am
Coll Cardiol. 2005; 46: 937-954.
- Roberts HR. Oscar Ranthoff: his contributions to the golden era of
coagulation research. Br J Haematol. 2003; 122: 180-198.
- Hoffbrand AV, Moss PAH, Pettit JE. Platelets, blood coagulation and
haemostasis.Haematology. 2008; 264-277.
- Paone G, Likosky DS, Brewer R, et al. Transfusion of 1 and 2 units of
red blood cells is associated with increased morbidity and mortality. Ann Thorac Surg. 2014; 97: 87-93
- Jeffrey R, Schears GJ, Nuttall GA, Oliver WC, Ereth MH, et al. Coagulation Parameter Thresholds Associated with Non-Bleeding in
the Eighth Hour of Adult Cardiac Surgical Post-Cardiotomy Extracorporeal Membrane Oxygenation. J Extra Corpor Technol. 2016;
48: 71-78.
- Jubelirer SJ, Mousa L, Reddy U, Mir M, Welch CA, et al. Coronary
artery bypass grafting (CABG) in patients with immune thrombocytopenia (ITP): a community hospital experience and review of the
literature. W V Med J. 2011; 107: 10-14.
- Vamvakas EC, Carven JH. RBC transfusion and postoperative length
of stay in the hospital or the intensive care unit among patients
undergoing coronary artery bypass graft surgery: the effects of
confounding factors. Transfusion. 2000; 40: 832-839.
- Haanschoten MC, van Straten AH, Verstappen F, van de Kerkhof
D, van Zundert AAJ, et al. Reducing the immediate availability of
red blood cells in cardiac surgery, a single-centre experience. Neth
Heart J. 2015; 23: 28-32.