Introduction
Since the introduction of endoscopic endonasal surgery for
skull base pathologies in the 1990s [1], increasing experience with
this technique has led to many progressive changes in patient
positioning, technique, and assessment in the operating room.
In addition, new surgical instruments have been developed for
endoscopic endonasal skull base surgery. We present our experience and assessment of the operating room.
Materials and methods
We report our experience in assessing the operating room and
surgical instruments in the last 218 endoscopic endonasal skull
base procedures.
Results
Operating room assessment: For the first procedures, preparation of the operating room was time-consuming. Over time, we
standardised the position of all devices (Table 1). After intubating
the patient, we positioned the magnetic flat-panel emitter under
the patient’s head and performed magnetic neuronavigation. We
never used a Mayfield head holder so that we could move the
patient’s head if necessary.
Position of the patient: The patient is positioned supine, in
neutral head position for pituitary surgery, in extended head posi tion for anterior fossa surgery, and in hyperflexive head position
for clivus and craniovertebral junction surgery. We drape the entire body except the nose and right paraombelical abdomen if we
need autologous fat.
Endoscope holder: Prior to surgery, an 800-bar pneumatic
high-power holder arm (Mitaka) is placed on the left side of the
patient and attached to the operating table with a light adapter,
then it is covered with a punctum holder drape. We alternate between the freehand and endoscope holder techniques as needed,
but for deeper procedures, such as sellar, suprasellar, and parasellar, we prefer the endoscope holder to have a fixed endoscope
and operate safely with both hands. Especially in long procedures,
the pneumatic endoscope holder helps and improves ergonomics
in neurosurgical endoscopic procedures. In our experience, the
endoscope holder has also proven to be very helpful during 3D
procedures.
Endoscopic equipment: The endoscopic column is positioned
in front of the surgeons, with two screens for the surgeons and for
the nursing staff and anesthesiologist. 0, 30, 45 and 70 degree, 4
mm diameter and 18 cm length rigid Storz endoscopes have been
used. In the last 8 procedures, we have had our experience with
3D endoscopes. A foot pedal irrigation system is always used to
clean the surgical field during the procedure. Instruments were always inserted along the endoscope for the two-nostril, two-three
and four-hand technique.
Position of surgeons: Surgeons are positioned in front and to
the side of the patient’s head.
They work under observation of endoscopic screens. Ultra-sound aspiration, laser and coagulation systems are positioned
above the patient’s feet.
Surgical tools: Bayonet instruments used in microsurgical techniques have been replaced by straight instruments so that they
can be inserted along the endoscope and rotated in all directions.
The tip of many instruments is the same as in microsurgical pituitary surgery, except for some tools and curved instruments.
In the endoscopic technique, there is a narrow working space,
so the classic bipolar coagulation often cannot be used, but a special bipolar punch can be used. We perform endonasal coagulation with monopolar suction coagulation and more recently with
the Tallio laser. The Tallio laser is a very effective tool for many
neurosurgical procedures and brings many improvements in endoscopic surgery, especially in hypertrophic turbinates, polipathologies, nasoseptal flaps and dural coagulation and cutting.
Discussion
The introduction of endoscopic endonasal surgery in the early
1990s [1,2] suddenly showed the possibility of approaching pituitary patology with many advantages over microsurgical procedures. In fact, the microsurgical procedure was performed with
a microscope outside the surgical field, looking forward through
a long tunnel (speculum) and finally seeing the sella turcica. No
view was possible outside the nasal speculum. The endoscope
is inserted into the surgical field and can be advanced as far as
the surgeon needs. We can reach any approach and always look
around the corners, with the ability to use an angled endoscope
and increase the view of the surgical field.
With this new perspective, we soon found that it was possible
to reach not only the sellar region, but the entire skull base contents in the nose. So we did a lot of anatomical studies. Thank
you to the great laboratory of Professor Manfred Tschabitscher at
the College of Vienna, we did many cadaveric studies [3,4]; then
in Pittsburgh, together with Dr. Jho, we studied and showed the
anatomy of the cavernous sinus with different endoscopic surgical approaches [5-7]; and with Prof. Tschabitscher and Dr. Jho,
we were the first in the world to show that the ventral craniovertebral junction, C1 and C2 could be reached by an endoscopic
endonasal approach [8,9]. All these anatomical studies opened
new important perspectives, and today these operations are routinely performed in most endoscopic skull base centers around
the world.
Even though the endoscopic technique has broadened the
indications for endonasal skull base pathology, this technique always requires a previous cadaveric study in the laboratory in order
to have a precise knowledge of the anatomy from an endonasal
point of view. Since the first procedures, we have learned to deal
with intraoperative hemorrhage. Intraoperative hemorrhage can
be frustrating because the surgeon cannot see anything during
the procedure. Therefore, close collaboration with the anesthesiologist is essential. We use local nafazoline and ropivacaine-cottonoid, without epinephrine. The anesthesiologist provides controlled hypotension and good analgesia. For carotid hemorrhage
and intracranial hemorrhage, we use Floseal and carotid neck compression. In the initial procedures, the surgeon must learn to
move the endoscope gently in the nose to reduce nasal hemorrhage by performing precise movements to reduce bleeding and
operative time. Multitasking instruments are very useful in this
operation. An aspiration coagulation system is always used, and
recently the introduction of the tallium laser has improved coagulation efficiency. The tallium laser is suitable for coagulation and
incision during the nasal and endosellar periods and proves to be
very efficient in coagulation and incision of the dura sellaris. Both
instruments complement each other, shortening surgical time
and improving outcomes and surgical comfort during surgery.
Many improvements have been made as the technique has
evolved. Since the first procedure, a Mayfield head holder has not
been used, allowing the head to be moved as needed during the
procedure. Magnetic neuronavigation with a flatter transmitter
under the patient’s head has always been used so that the head
can be free of any reference frame. Mitaka’s pneumatic endoscopy holder is very useful. It is very easy to maneuver, but once it
is fixed, it is very stable. This tool is very useful because it allows a
wide range of positions and can always be placed in both nostrils
with a comfortable and plastic movement without fatigue of the
surgeon. The presence of the Mitaka holder improves the space
for hand movements in a very narrow surgical field.
In this procedure, it is important to improve ergonomic principles [10]. Xu et al. reviewed 50 articles on ergonomics in endoscopic skull base surgery to highlight the importance of adopting
best practices. Even though the endoscopic procedure is less invasive and traumatic for patients, it is technically challenging for
surgeons.
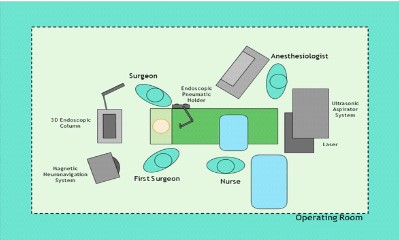
The assessment of the operating room must be carefully
planned beforehand. In figure 1, we have shown our surgical planning for endoscopic endonasal skull base surgery.
Teamwork is very important to optimize preoperative and operative times. After anesthesia, all technical devices were placed.
First, magnetic neuronavigation planning is performed. The neuronavigation screen is placed in front of the surgeon on the left
side. Then the pneumatic endoscope holder is placed to the left
of the patient. The endoscope column with two screens is placed
in front of the surgeon. Disinfection of the surgical field (nose and
right paraombelical region) and draping of the patient are performed. The endoscope holder is covered with a special sterilization device.
The first surgeon is placed on the right side of the patient, and
the second surgeon is placed on the left side. In the endonasal
phase of the procedure, we usually use the freehand endoscope
technique, and if we have enough space, usually after opening
the sphenoid sinus we attach the endoscope to the pneumatic
holder to have both hands free and to reduce surgeon fatigue and
the risk of accidental mishandling. We have found this technique
to be very helpful and can change the procedure at any time. In
the last 8 procedures, we have used 3D endoscopes in endosellar
and intracranial phases. Once the endoscope is attached to the
mount, the surgeon doesn't have to change the screen. This is because with 3D glasses, it can be very uncomfortable to look from
the screen to the nose or the surgical field. We found the combination of the endoscopy holder and 3D endoscopy very helpful (Figure 2). The 3D view was very helpful in improving depth
perception and preserving important neurovascular structures.
Depth perception is the limit of the 2D camera, and with the 3D
endoscope we can now overcome this limit [11]. In the intracranial phase of the procedure, we found the 3D vision very useful,
similar to microscope vision and with the possibility of a really
similar microscopic procedure.
Conclusions
Endoscopic endonasal skull base surgery is still a difficult procedure. Many improvements have been made over the years, but
the ergonomics and surgical instruments aren’t yet mature. In our
experience, accurate assessment of the operating room improves
surgical ergonomics and surgical outcomes. The pneumatic endoscope holder has been routinely used since 2010 because it
reduces surgeon fatigue and improves precise two-, three-, and
four-handed procedures in a very narrow surgical field. In addition, the endoscope holder is very useful in 3D endoscope procedures because the surgeon doesn’t have to move the 3D glasses
from the screen to the patient’s nose to insert and move the free-hand endoscope technique. The 3D technique has been used in
the last 8 procedures and has improved our depth perception,
with a true microscope-like view and better control of the lesion
and neurovascular structures.
References
- Jho HD, Carrau RL. Endoscopic endonasal transsphenoidal surgery:
experience with 50 patients. J Neurosurg. 1997; 87(1): 44-51.
- Jho DH, Jho DH, Jho HD. Early Development of Endoscopic Endonasal Pituitary and Skull Base Surgery. Global Journal of Otolaryngology ISSN 2474-7556. 2018; 15(4).
- Atlas of endoscopic anatomy for endonasal intracranial surgery.
P. Cappabianca, A. Alfieri, E. de Divitiis, M. Tschabitscher (eds).
Springer Verlag, Wien, 2001.
- Alfieri A. Endoscopic endonasal transsphenoidal approach to the
sellar region. Technical evolution of the methodology and refinement of a dedicated instrumentation. J Neurol Sci. 1999; 43: 85-92.
- Jho HD, Alfieri A. Endoscopic Transsphenoidal Pituitary Surgery:
various surgical technique and recommended steps for procedural
transition.Br J Neurosurg. 2000; 14 (5): 432-40.
- Alfieri A, Jho HD. Endoscopic endonasal cavernous sinus surgery:
an anatomic study. Neurosurgery. 2001; 48: 827-837.
- Alfieri A, Jho HD. Endoscopic endonasal cavernous sinus surgery:
surgical approaches. Neurosurgery. 2001; 49: 354-362.
- Alfieri A, Jho HD, Tschabitscher M. Endoscopic endonasal approach to the ventral cranio-cervical junction. Acta Neuroch. 2002;
144: 219-225.
- Alfieri A, Jho HD, Schettino R, Tschabitscher M. Endoscopic endonasal approach to the pterygopalatine fossa: anatomic study. Neurosurgery. 2003; 52: 374-380.
- Xu C, George Hanna, Brendan M Fong, Frank PK Hsu, Gilbert Cadena, Edward C Kuan. Ergonomics of endoscopic skull base surgery: a
systematic review. 2020.
- Guo Xin, Yajing Liu, Yicheng Xiong, Shenhao Xie, Hai Luo, Liming
Xiao, Xiao Wu, Tao Hong and Big Tang. The use of three-dimensional endoscope in transanasal skull base surgery: a single-center
experience from China. Front. Surg. 2022; 9.