Introduction
Necrotising Fasciitis (NF) is a bacterial infection of fascia leading
to necrosis of skin, subcutaneous tissue and superficial fascia. This
is a rare, rapidly progressing, potentially fatal infection. It spreads
rapidly across fascial planes. In spite of newer diagnostic tools
and management, the mortality rate is still high in the range of
approximately 25% [1]. Most commonly involved areas are groin,
abdomen and extremities [2]. Necrotising fasciitis of perineum
and genitalia is referred to as “Fournier’s gangrene.” Necrotising
fasciitis of the breast is extremely rare. Mortality rates have been
reported as high as 73%, but can be reduced with early diagnosis
and prompt institution of appropriate management strategies [3].
Late presentation as well as misdiagnosis, often leads to a total
mastectomy or life-threatening outcomes.
Case report
A 37-year-old patient on vacation to India developed left breast
pain with tenderness of a short duration. A diagnosis of breast
abscess was made after appropriate evaluation. Incision & Drainage of the abscess was done and she was put on antibiotics. She
continued to have symptoms with rapid progression and discoloration of skin. On examination, left breast was enlarged, tender,
oedematous with erythema and necrotic patches on the skin. Left
axillary lymph nodes were enlarged. She was a diabetic, on oral
hypoglycaemic agents. Lab investigations showed elevated total
count 14.03 x 10 with neutrophil count 4.3 x 10, ESR of 103 mm/hr
and CRP was positive (427).
Ultrasound scan revealed diffuse skin thickening, subcutaneous oedema and bright echoes in the glandular parenchyma possibly due to air pockets degrading the image quality and hence
the visualization of deeper tissues was suboptimal.
CT scan was done to assess the extent of involvement, which
revealed diffuse air pockets confined to the glandular parenchyma of left breast with minimal air in the superficial intermuscular
plane. There was no involvement of chest wall muscles. CT scan
along with clinical examination confirmed the diagnosis of necrotising fasciitis. Surgical exploration showed extensive necrotic tissues, spreading into the abdominal wall and hence total mastectomy was done.
Gross specimen showed blackish discoloration on the skin surface measuring 9 x 6 cm with another area of ulceration measuring 5 x 2.5 cm. Serial sectioning of the breast showed scattered
ill-defined necrotic areas.
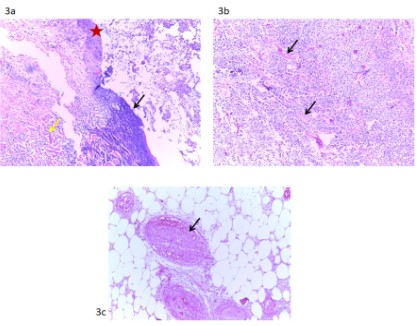
Multiple sections from the breast showed a large abscess
cavity with intense inflammation, extensive tissue necrosis with
necrotic debris, and prominent intravascular thrombosis. The necrosis extends along deep dermis and adipose tissue with involvement and ulceration of overlying epidermis. The inflammatory
infiltrate predominantly consists of neutrophils and macrophages
with diminished lymphocytes, plasma cells and eosinophils. The
inflammatory cell infiltrate was seen between and enveloping the
adipocytes. Dermis shows necrotic collagen. Histopathology was
consistent with necrotizing fasciitis, involving almost the entire
breast and axillary fat, extending up to the margins.
Pus sample from left breast was sent for microbiological analysis. Gram stain showed plenty of pus cells along with occasional Gram negative bacilli and few Gram positive cocci in clusters
which on culture grew Proteus mirabilis.
Postoperatively, she was put on IV antibiotics. Her postoperative period was uneventful.
Discussion
Necrotising fasciitis is a rare but serious rapidly progressive
infection characterised by widespread necrosis of subcutaneous
tissue and fascia with associated systemic toxicity. It is extremely
rare in breast and first case of necrotising fasciitis of breast is reported by Shah et al [4]. In the breast, it is usually a unilateral
rather than a bilateral infection.
Predisposing factors for the development of necrotising fasciitis include surgical procedures, trauma, minor cuts and burns,
and the disease is more common in patients who have diabetes
mellitus, peripheral vascular disease or who are immunosuppressed.
It is characterised by widespread fascial necrosis with relative
sparing of skin and muscle, and occurs more commonly in patients with comorbidities.
Introduction of the pathogen into the subcutaneous space
occurs via disruption of the overlying skin or by hematogenous
spread from a distant site of infection. Polymicrobial necrotizing fasciitis is usually caused by enteric pathogens, whereas mono-microbial necrotizing fasciitis is usually due to skin flora. Tissue
damage and systemic toxicity are believed to result from the release of endogenous cytokines and bacterial toxins [5]. Based on
aetiology necrotizing fasciitis can be classified as Type I, II, or III
[6]. NF is typically a polymicrobial infection, caused by a diverse
group of bacteria, both aerobic and anaerobic - including Group A
B-hemolytic streptococci, Staphylococcus aureus, Escherichia coli,
Clostridium spp, and Bacteroides species. Usually the causative
agents are introduced via traumatic or surgical insult and this
class of NF typically occurs in the perianal and abdominal areas.
Type II NF is due to monomicrobial infection with Group A B-hemolytic streptococci, and most often affects the extremities. This
type is frequently found in high-risk patients i.e, diabetic, obese,
immunocompromised and patients with peripheral vascular disease. The final Type III NF is uncommon and refers to infection
caused by Vibrio vulnificus, which may be transmitted to humans
by fish or marine insect and some authors refers this as necrotizing clostridial infections [7]. The causative organism in our patient
was proteus mirabilis.
Initially, patients generally present with flu-like symptoms,
diarrhea, thirst, and gastric symptoms. The lesion appears red,
shiny, tense, and oedematous with no clear border. It is not easy
to differentiate from cellulitis in the early stage. Severe pain out
of proportion to the apparent severity of the lesion should alert
the physician to the possibility of NF because early diagnosis and
treatment is crucial to increase the chance of survival [8,9].
Systemic findings, such as high fever, chills, hypotension, and
multiple organ failure, may appear as toxins are released into the
blood and bacteraemia advances to sepsis or when superimposed
by streptococcal toxic shock syndrome [10].
The diagnosis is usually challenging and is made based on the
combination of clinical, cultural, laboratory, as well as imaging
finding.
Laboratory results show normocytic, normochromic anaemia;
elevated total count with left shift; elevated erythrocyte sedimentation rate.
Elevated serum creatinine levels along with haemoglobinuria
indicates renal involvement; increased serum creatine kinase levels indicate muscle involvement. Extensive fat necrosis may result
in hypocalcaemia [11,9].
Blood culture and Gram stain of infected tissue can help identify the causative organisms and aid in the choice of antibiotics.
Biopsy with frozen section shows massive infiltration of fascia
by polymorphonuclear leukocytes, which facilitates an early diagnosis and treatment.
Imaging modalities, i.e., ultrasound (USG), CT, and MRI scans
are used to aid the diagnosis. Ultrasound findings usually reveal
oedematous thickening of the fascia associated with fluid collections or air. Tsai et al. have described the sonographic finding of
necrotizing fasciitis as irregularity of the fascia, abnormal fluid
collections along the fascial planes, and diffuse thickening of the
fascia [12]. On CT, gas within fluid collections tracking along fascial planes is the most specific finding but is not always present
[13]. Other, non-specific findings include fascial thickening associated with fat stranding, oedema extending into the intermuscular
septa and the muscle, thickening of one or both of the superficial
and deep fascial layers. Although fascial fluid collections are typically non-focal, abscesses may be seen. In 2012, Kaczynski et al.
first reported gas in the subcutaneous tissue of the breast in a
75-year-old patient [14]. Although MRI has a low specificity of 46-86%, it can reveal the extent of deep tissue involvement in more
detail than any other imaging modality [14]. MRI is superior to CT
in differentiating healthy and necrotic tissue. Even though imaging is a useful adjunct in establishing the diagnosis, it should not
cause delay in delivering definitive care. Detection of gas in CT has
got high specificity but low sensitivity to diagnose NF. MRI is time
consuming and may not be readily available [15]. There is difference between the necrotising fasciitis of breast and other organs.
Because of thick tissue between skin and deeper tissue, the cutaneous symptoms occurs late and by that time the breast may
not be salvageable. Because of bridge between deeper tissue of
contralateral breast, infection can rapidly spread to opposite side,
this is the reason for bilateral involvement of necrotising fasciitis
of breast.
Direct inspection of the fascia by surgical exploration is the
fastest way to arrive at the diagnosis [16]. Pus between the fascial
planes or necrotic tissue may be seen, and easily separable fascial
planes during surgical exploration is almost pathognomonic for
NF.
The main principles of treatment are broad-spectrum antibiotics with debridement of the necrotic tissue and supportive care.
Emergency surgery is warranted if symptoms are severe, if no response to treatment for presumed cellulitis is observed for 1 or 2
days, or if signs suggesting NF over cellulitis, such as gas in imaging tests, are seen. In the operating room, extensive surgical de-
bridement and fasciotomy are essential [17]. After initial debridement, repeated debridement may be performed as needed. Skin
and muscle grafts may be required after the infection is cleared.
Supportive care in an intensive care unit should include fluid replenishment and nutritional support with sufficient calories, proteins, and vitamins C and E.
Necrotizing fasciitis of the breast is a rare disease which carries
significant morbidity to the patients. Early diagnosis and surgical
debridement prevails to be the mainstay of treatment and patients generally respond well with adequate debridement.
Conclusion
Necrotizing fasciitis of the breast can be a rapidly progressive
and fatal entity if appropriate treatment is not initiated at the earliest. Prompt diagnosis and rapid surgical intervention is crucial
to prevent mastectomy and fatal outcome. Clinical examination
along with imaging finding can guide the clinician to reduce the
mortality in these critically ill patients.
Statement and declarations
Conflicts of interest/Competing interests: None
Financial interests: The authors have no relevant financial interests to disclose.
Non-financial interests: The authors have no relevant non-financial interests to disclose.
Availability of data and material: No data available
Compliance with Ethical standards: Compliant.
Author contributions: All authors contributed to the study
conception and design. The first draft of the manuscript was written by Dr Dhanya Jacob and all authors commented on previous
versions of the manuscript. All authors read and approved the final manuscript.
References
- Singh G, Sinha SK, Adhikary S, Babu KS, Ray P, et al. Necrotising
infections of soft tissues—a clinical profile. European Journal of
Surgery. 2002; 168: 366-371.
- Fontes Jr RA, Ogilvie CM, Miclau T. Necrotizing soft-tissue infections. JAAOS-Journal of the American Academy of Orthopaedic
Surgeons. 2000; 8: 151-158.
- Suresh Kumar D, Viswanathan MP, Navin Noushad S, Anandh SM.
Necrotizing fasciitis of cancer breast: case report and literature review. Indian Journal of Gynecologic Oncology. 2020; 18: 58.
- Shah J, Sharma AK, Johri A, Mearns B, O’Donoghue JM, Thomas
VA. Necrotising fasciitis of the breast. British journal of plastic surgery. 2001; 54: 67-68.
- Green RJ, Dafoe DC, Rajfin TA. Necrotizing fasciitis. Chest. 1996;
110: 219-229.
- Ward ND, Harris JW, Sloan DA. Necrotizing fasciitis of the breast
requiring emergent radical mastectomy. The Breast Journal. 2017;
23: 95-99.
- Salcido RS. Necrotizing fasciitis: reviewing the causes and treatment strategies. Adv Skin Wound Care. 2007; 20: 9-11.
- Wong CH, Wang YS. The diagnosis of necrotizing fasciitis. Current
opinion in infectious diseases. 2005; 18: 101-106.
- Kihiczak GG, Schwartz RA, Kapila R. Necrotizing fasciitis: a deadly
infection. Journal of the European Academy of Dermatology and
Venereology. 2006; 20: 365-369.
- Elliott DC, Kufera JA, Myers RA. Necrotizing soft tissue infections.
Risk factors for mortality and strategies for management. Annals
of surgery. 1996; 224: 672.
- Kessenich CR, Bahl A. Necrotizing fasciitis: Understanding the
deadly results of the uncommon ‘flesh-eating bacteria.’. AJN The
American Journal of Nursing. 2004; 104: 51-55.
- Hanif MA, Bradley MJ. Sonographic findings of necrotizing fasciitis
in the breast. Journal of Clinical Ultrasound. 2008; 36: 517-519.
- Marks B, Fasih T, Amonkar S, Pervaz M. Necrotising fasciitis of the
breast: a rare but deadly disease. International journal of surgery
case reports. 2019; 65: 10-14.
- Kaczynski J, Dillon M, Hilton J. Breast necrotising fasciitis managed
by partial mastectomy. Case Reports. 2012; 2012: bcr0220125816.
- Cai Y, Cai Y, Shi W, Feng Q, Zhu L. Necrotizing fasciitis of the breast:
a review of the literature. Surgical Infections. 2021; 22: 363-73.
- Stone DR, Gorbach SL. Necrotizing fasciitis: the changing spectrum. Dermatologic clinics. 1997; 15: 213-266.
- Meltzer DL, Kabongo M. Necrotizing fasciitis: a diagnostic challenge. American Family Physician. 1997; 56: 145-149.