Introduction
ABC is mostly primary and can occur in any part of the body. It
is more common in the epiphysis of the long shaft, mostly on the
surface of the bone. The huge ABC of the femoral head is relatively
rare [1]. For the treatment of ABC, debridement and bone grafting
are often used, but arthroscopy is rarely used β-Tricalcium phosphate bioceramic rod in the treatment of femoral head ABC. The
authors used arthroscopic debridement and compression bone
graftceramic rod implantation in the treatment of 1 case of huge
ABC of the femoral head. The patients were followed up for 1 year
and achieved good results.
Case data
Medical history and examination patient Luo Moumou, a 26
year old civil servant, was hospitalized for 3+ months due to left
hip pain. Physical examination: No redness, swelling, bruise, etc.
in the left hip, the skin color is not red and the skin temperature
is not high. The four character test was positive, the Thomas test
was negative, the left hip was active, and the superficial lymph
nodes were not enlarged. Previous health, family genetic history,
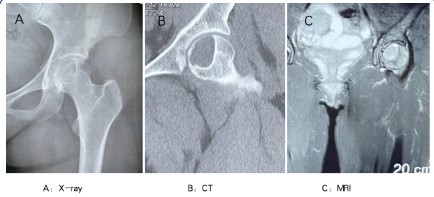
trauma and surgery history, parents’ and brothers’ health. Laboratory examination showed no special, tumor markers and tuberculosis antibody were negative. X-ray showed cystic changes in
the left femoral head, normal joint space, and acceptable femoral
head morphology. CT findings showed that the cystic hypodense
area of the left femoral head was septate, with sclerotic marginal
bone and thin medial marginal bone cortex. MRI showed that the
left femoral head was cystic, short T1 and long T2, with layered
changes, with low signal ring at the edge, intact cortical bone
shell, diffuse edema of surrounding bone marrow, and no abnormality in joint soft tissue (Figure 1).
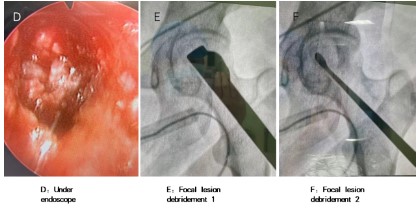
During the operation process and intraoperative findings, the
patient was placed in a supine position, the left hip was padded
10 cm high, the left hip and left lower limb were covered with a
conventional disinfection towel, and the lateral side of the proximal femur was exposed. Under fluoroscopy, the guide pin was
placed to the center of the femoral head and neck, about 10 mm
from the articular surface, and the femur was perforated. The
cancellous bone debris of the neck was collected and drilled into
the femoral head tumor cavity to establish a channel. Arthroscopy
showed a large number of tumor like hyperplasia in the lesion,
which was blood like. A scraper was placed under fluoroscopy,
and the lesion was cleared to normal bone and local micro bleeding. The curved curette was used to clean up the local residual lesions again. After the lesions were completely cleaned under the
microscope, the tumor cavity was inactivated by radiofrequency
ablation, and the flushing tube was placed to rinse with normal
saline. β-Tricalcium phosphate bioceramic particles mixed with
autologous cancellous bone debris were used for femoral head
lesion compression bone graft. After the bone graft was found to
be appropriate under fluoroscopy, ceramic rods were implanted
for head and neck channel occlusion (Figure 2).
X-ray examination after operation and follow-up showed that
the lesions of the femoral head were completely removed and
the bone graft filling was acceptable. On the first day after the
operation, the patient was instructed to help both crutches to the
ground, and the affected limb was not loaded, and the patient
was instructed to perform postoperative functional exercise. Post-operative pathological examination: HE staining ×100 see more
homogeneous red stained cellulose like substances,and aneurysmal bone cyst was diagnosed. Three months after the operation,
the follow-up X-ray showed that the osteogenesis in the original
lesion was good, and there was no significant change in the joint
space. Ask the patient to change the single crutch to assist walking, and carry some weight on the affected limb. After 6 months
of follow-up, the patient did not complain of left hip pain and
discomfort, and the joint function was good. The patient was instructed to abandon the crutch and walk without assistance. X-ray
reexamination showed that cystic lesions disappeared and bone
graft grew well. The reexamination of MRI showed patchy long
T1 and long T2 signals of the left femoral head, and no abnormal
signals were found in the surrounding soft tissue (Figure 3).
Discussion
ABC is often considered to be a benign lesion. Its etiology is
not very clear, but it may be related to trauma and heredity. Some
scholars believe that ABC may be formed by the blood infiltrating into bone cyst after the increase of venous pressure [2]. Its
clinical manifestations are often atypical [3], mostly because of
joint pain with limited activity, and the pain is mainly intermittent
pain. When ABC occurs in the superficial bone, it may touch the
mass, and larger ABC may lead to pathological fracture. The typical imaging changes were cystic and expansive bone destruction
with intact bone capsule, mostly central destruction, and a few
eccentric and lobulated. The formation of liquid-liquid plane can
be seen in MRI, soft tissue mass can appear, surrounding bone
can have edema reaction, and a few may have buttress periosteal
reaction [4]. Imaging examination should be distinguished from
simple bone cyst, giant cell tumor of bone, abnormal proliferation
of bone fibers, etc. [5]. The pathological changes of primary ABC
were mostly hyperemic cavities without epithelial lining, and the
cyst septal boundary was composed of fibroblasts and myofibroblasts. Secondary ABC imaging and pathological atypical are difficult to diagnose [6,7]. Detection of usp6 gene rearrangement by
fish plays an important auxiliary role in the pathological diagnosis
of cases with atypical clinical pathological manifestations [8,9].
For the treatment of ABC, focus clearance and bone graft after tumor cavity inactivation are advocated. When the lesion is in
the active and invasive stage, the postoperative recurrence rate
is high [10]. The lesions were removed as much as possible during the operation to reduce the recurrence rate. Clinically, ethanol
and electric knife cauterization are often used to inactivate the
ABC tumor cavity of the femoral head, which is difficult to operate. During the operation, the lesion was removed with a scraper
and curette, and the tumor was completely removed under the
microscope, and then inactivated by radiofrequency ablation.
Zarzour OA et al. [11] used radiofrequency ablation to inactivate
the tumor in bone tumors with good effect. Arthroscopic debridement is less invasive, faster recovery and more conducive to complete debridement. AIBA h et al. [12] used endoscopic minimally
invasive technology to treat ABC with satisfactory curative effect.
In addition, the destruction of articular cartilage should be avoided during operation to avoid affecting joint function as much as
possible. The stress of the femoral head and neck is large, and
the huge ABC is prone to pathological fracture, so internal fixation can be used to prevent postoperative fracture [13]. There are
relatively few reports on femoral head and neck ABC. Ndour o et
al. [14] used femoral neck lesion removal, bone graft and screw
internal fixation to treat a case of femoral neck ABC with satisfactory effect. Scholars at home and abroad generally believe that
internal fixation combined with debridement and bone graft can
be used to treat bone tumors in the femoral head and neck [15].
Bioceramic is a kind of bioactive ceramic material with biodegradability, good biocompatibility and bone conductivity. It is an
ideal bone defect repair material [16,17]. In recent years, it has
been widely used in spinal and vertebral fusion and limb bone
defect repair. It has also been reported at home and abroad that
it is used to fill bone graft after the removal of femoral head necrosis lesions [18]. This case is ABC in the weight-bearing area
of the femoral head. The subchondral bone is thin. After the lesion is cleared, the remaining bone mass loses its structural support ability. Even if the weight-bearing of the hip joint is avoided,
there is a risk of collapse of the femoral head when moving the
hip joint. Intraoperative application β- Tricalcium phosphate bioceramics mixed with autologous cancellous bone graft, β- The mechanical strength of tricalcium phosphate bioceramics is greater
than 2MPa, which can provide certain mechanical support in the
lesion area, and its degradation rate matches the rate of new
bone formation, which can effectively prevent the collapse of the
femoral head [19]. The neck bone tunnel is blocked with ceramic
rods, which not only provides a certain effective support, but also
avoids the disadvantages of secondary internal fixation such as
femoral neck dynamic cross nail.
To sum up, the author used arthroscopic debridement and
compression bone graft + ceramic rod implantation in the treatment of huge ABC of the femoral head, and achieved good results.
However, the minimally invasive surgery is not suitable for all benign lesions of the femoral head, such as lesion erosion of the
articular surface, collapse of the femoral head, lesions larger than
2/3 of the femoral head, and other open surgical treatments such
as joint replacement may be required.
Declarations
About the author: Huang yanchang (1986-), male, doctor,
deputy chief physician, whose main research field is the direction
of joint orthopedics of integrated traditional Chinese and Western medicine, email: 250973069@qq.com Detailed address: Department of Orthopaedics, Second Affiliated Hospital of Guizhou
University of traditional Chinese medicine, No. 83, Feishan street,
Yunyan District, Guiyang, Guizhou Province, Tel: 0851-85559113,
mobile: 13765818867
Fund Project: Basic research project of Guizhou Provincial Department of science and technology: Guizhou Kehe foundation
zk(2022) general 479; The Second Affiliated Hospital of Guizhou
University of traditional Chinese medicine's green seedling research startup Fund Project: gzeyk (2022) No. 8; Internal medicine
research project of the Second Affiliated Hospital of Guizhou University of traditional Chinese medicine: gzeyk (2020) No. 2, gzeyky (2021) No. 5; Internal research project of Guizhou University of
traditional Chinese medicine in 2019: Guizhong Medical College
(2019) No. 27.
References
- Shooshtarizadeh T, Movahedinia S, Mostafavi H, Jamshidi K, Sami
SH. Aneurysmal Bone Cyst: An Analysis of 38 Cases and Report of
Four Unusual Surface Ones. Arch Bone Jt Surg. 2016; 4: 166-72.
- Ye Y, Pringle LM, Lau AW, Riquelme DN, Wang H, Jiang T, Lev D,
Welman A, Blobel GA, Oliveira AM, Chou MM. TRE17/USP6 oncogene translocated in aneurysmal bone cyst induces matrix metalloproteinase production via activation of NF-kappaB. Oncogene.
2010 Jun 24; 29(25): 3619-29.
- Johnson EM, Caracciolo JT. Solid variant aneurysmal bone cyst in
the distal fibular metaphysis: radiologic and pathologic challenges
to diagnosis. Radiol Case Rep. 2017; 12(3): 555-559.
- Restrepo R, Zahrah D, Pelaez L, Temple HT, Murakami JW. Update
on aneurysmal bone cyst: pathophysiology, histology, imaging and
treatment. Pediatr Radiol. 2022; 52(9): 1601-1614.
- Kelly D, Mc Erlean S, Byrne D, Mahon PM, Mc Caffrey J. A case
of thoracic giant cell tumor of bone and discussion of radiological features and current management practices. Radiol Case Rep.
2016; 11(3): 222-6.
- Song W, Suurmeijer AJH, Bollen SM, Cleton-Jansen AM, Bovée
JVMG, Kroon HM. Soft tissue aneurysmal bone cyst: six new cases
with imaging details, molecular pathology, and review of the literature. Skeletal Radiol. 2019; 48(7): 1059-1067.
- Jalan D, Gupta A, Elhence A, Nalwa A, Bharti JN, Elhence P. Primary
aneurysmal bone cyst of the calcaneum: A report of three cases
and review of literature. Foot (Edinb). 2021; 47: 101795.
- Blackburn PR, Davila JI, Jackson RA, Fadra N, Atiq MA, Pitel BA, Nair
AA, VanDeWalker TJ, Hessler MG, Hovel SK, Wehrs RN, Fritchie KJ,
Jenkins RB, Halling KC, Geiersbach KB. RNA sequencing identifies a
novel USP9X-USP6 promoter swap gene fusion in a primary aneurysmal bone cyst. Genes Chromosomes Cancer. 2019; 58: 589-594.
- Mejbel HA, Zein-Sabatto B, Wei S, Siegal GP. An Aneurysmal bone
cyst harboring a novel ACSL4::USP6 fusion gene. J Orthop Sci. 2023
Jun 20:S0949-2658(23)00143-4.
- Muratori F, Mondanelli N, Rizzo AR, Beltrami G, Giannotti S, Capanna R, Campanacci DA. Aneurysmal Bone Cyst: A Review of Management. Surg Technol Int. 2019; 35: 325-335.
- Zarzour OA, Santiago FR, Serrano NO, Abdallah AH, El-Sharkawy
MA, Mourad AF. CT-guided radiofrequency ablation in patients
with aneurysmal bone cysts. Eur J Radiol. 2018; 100: 116-123.
- Aiba H, Kobayashi M, Waguri-Nagaya Y, Goto H, Mizutani J, Yamada
S, Okamoto H, Nozaki M, Mitsui H, Miwa S, Kobayashi M, Endo K,
Saito S, Goto T, Otsuka T. Treatment of aneurysmal bone cysts using endoscopic curettage. BMC Musculoskelet Disord. 2018; 19(1):
268.
- Cha SM, Shin HD, Kim KC, Kang DH. Flexible intramedullary nailing
in simple bone cysts of the proximal humerus: prospective study
for high-risk cases of pathologic fracture. J Pediatr Orthop B. 2013;
220: 475-80.
- Ndour O, Boseba R, Damipi JB, Nibagora J, Fall AL, Ngom G, Ndoye
M. Aneurysmal femoral neck cyst: Report of a paediatric case and
review of literature. Afr J Paediatr Surg. 2016; 13: 103-106.
- Günther KP, Hartmann A, Aikele P, Aust D, Ziegler J. Large femoralneck cysts in association with femoroacetabular impingement. A
report of three cases. J Bone Joint Surg Am. 2007; 89: 863-70.
- Fillingham YA, Cvetanovich GL, Haughom BD, Erickson BJ, Gitelis S.
Bioceramic bone graft substitute for treatment of unicameral bone
cysts. J Orthop Surg (Hong Kong). 2016; 24: 222-7.
- Sethu SN, Namashivayam S, Devendran S, Nagarajan S, Tsai WB,
Narashiman S, Ramachandran M, Ambigapathi M. Nanoceramics
on osteoblast proliferation and differentiation in bone tissue engineering. Int J Biol Macromol. 2017; 98: 67-74.
- Quan H, Ren C, He Y, Wang F, Dong S, Jiang H. Application of biomaterials in treating early osteonecrosis of the femoral head:
Research progress and future perspectives. Acta Biomater. 2023;
164: 15-73.
- Chiba S, Anada T, Suzuki K, Saito K, Shiwaku Y, Miyatake N, Baba
K, Imaizumi H, Hosaka M, Itoi E, Suzuki O. Effect of resorption rate
and osteoconductivity of biodegradable calcium phosphate materials on the acquisition of natural bone strength in the repaired
bone. J Biomed Mater Res A. 2016; 104: 2833-42.